Diagnosis is the first step in getting better treatment plans. A Functional approach assesses the whole patient, considering underlying causes in a serious way. Functional medical thinking refuses to accept the presenting symptom as the entire picture. It leads to a diagnosis that is more holistic and more specific. The integrative approach then utilizes several treatment approaches to get a much more comprehensive set of treatment options. Integrative sports medicine asserts a true team approach, where the team synergistically employs the available skills, techniques and treatments, utilizing any or all parts of my skill-set, and most importantly any and all of the therapeutic community.
Bursitis
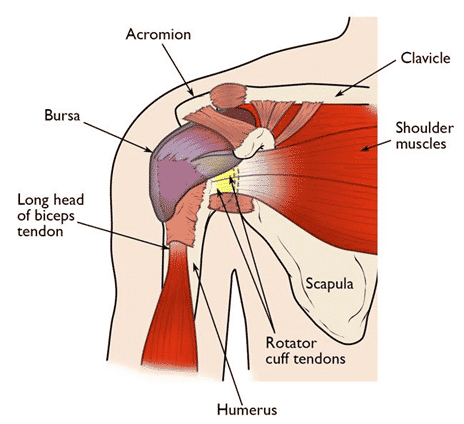
A bursa is a friction-reducing structure between two things in the body that move. It is a “potential space,” like a water balloon with just a tiny amount of lubrication inside so that whatever is attached to one side can freely glide against whatever is attached to the other side. I’ll give two examples. First, the subacromial bursa. This sits between the rotator cuff and the acromion bone at the top of the inside of the shoulder. It allows the rotator cuff, which moves a great deal, to glide by overlying structures such as the acromion bone, the end of the collarbone (clavicle) and the deltoid muscle, do not move much compared with the rotator cuff tendons.
Figure 1: Subacromial bursa of shoulder, Courtesy AAOS (see above)
A good second example would be any of the bursae around the greater trochanter, which collectively are called the “trochanteric bursa.” These bursae allow movement of the muscles overlying the greater trochanter against themselves and against the bone. The tensor fascia lata, has to glide against the iliotibial band, and both of these structures are muscles with a big, wide band of tendon. All the muscle-tendon units have to be able to glide over the greater trochanter. The trochanteric bursa allows this by greatly reducing the friction.
All bursae are subject to becoming inflamed, and typical medical advice includes icing, taking NSAIDs, and sometimes progression to corticosteroid injection and even surgical bursectomy.
My take is that all these therapies miss the point. They miss it because they assume that bursitis is the entity. To the contrary, bursitis is a side-effect. To get a diagnosis that can lead to a cure rather than a band-aid approach, integrative and functional medicine need to be employed.
Functional Medicine as the Basis of Diagnosis and Integrative Medicine as a System of Treatment
If you are reading this, I am guessing that you have a sense that there is something terribly wrong with how traditional medicine is being presented to you. You are right. It is not just the money machine, not just “Big Pharma” and not just the unreasonable time pressure your doctor faces. Traditional medicine is at times fundamentally flawed by cognitive errors which are sometimes intertwined with the system errors within medical bureaucracy. There are many cognitive errors in medicine (see https://www.jround.co.uk/error/reading/crosskerry1.pdf). Functional medicine is a step towards correcting some of these cognitive errors that lead to superficial or spurious diagnoses.
Functional medicine looks for underlying causes in a serious way. It’s not just “you contracted bursitis from overuse.” It is more like, “you contracted bursitis because the adjacent tendon/muscle use is under chronic strain due to an adverse biomechanical pattern, under-recovery, sub-optimal nutrition and other specific factors.” This gets to why bursitis should not just be squelched by a steroid injection, but the underlying reasons it happened in the first place should be addressed. Here is an example of how Functional thinking might occur in a certain patient with a subacromial bursitis.
- The patient has gotten “out of shape,” leaving the tendons adjacent to the bursa unhealthy.
- The person got “out of shape” because of work and life stressors that reached a breaking point, leading to the patient taking less time to rest, sleep and exercise;
- Because of time pressure and a shift of priorities from good health to making deadlines, good nutrition such as an exuberant intake of vegetables and a control on calorie intake went by the wayside.
- Because of the inadequate intake of micronutrients (vitamins in food) and rest, tendons are not able to heal from day to day.
- Because the tendons are under stress, the patient takes NSAIDs (non-steroidal anti-inflammatory medications) to deal with the pain. The NSAIDs compound the problem by blocking an “inflammatory” biological pathway in connective tissue healing. This compounds the underlying tendon healing problem.
- Because the patient realizes they are “out of shape” they start exercising, but not with good form and beyond their current ability level, thinking about an earlier era in their life when certain effort and repetitions did not lead to problems. They do military overhead presses which stress the rotator cuff tendons in the shoulder and mechanically damage them by impinging on the acromion bone.
- Because of the impingement, under-nutrition and under-recovery, the rotator cuff tendons begin to develop micro-tearing.
- Because of the micro-tearing, the rotator cuff tendons develop micro-tearing of their collagen sub-units, the collagen fibrils. If I am lucky enough to see the patient at that point, I can see these small injuries on in-office diagnostic ultrasound and address the problem before it progresses to a rotator cuff tear.
- Because tendon micro-tears don’t hurt badly at first, all the above processes continue unabated.
- Because the patient is un-aware of an impending problem, they continue to do military overhead presses, and the impingement problem is ever-worsening due to the progressively bad biomechanics that results from a sub-optimal rotator cuff.
- Eventually micro-tears of the rotator cuff release enough inflammatory mediators that the sub-acromial bursa becomes inflamed. In addition, by this point, there is likely a partial tear of the rotator cuff.
- The point of this is that the “bursitis” is not an isolated inflammation of the bursa that came out of no-where. It is a result of the adjacent tendons trying to heal from chronic micro-tearing.
At this point, most clinicians are trained and time-pressured to identify and “treat” the bursitis. They are using System 1 thinking, the immediate, emotional response of what seems right (see https://bigthink.com/errors-we-live-by/kahnemans-mind-clarifying-biases for a quick look at that). Then the doctor might jump right to “inject the bursa with steroid” (unintentionally by often harmful) and move on with the day. In contrast, the Functional approach is to consider all 11 (and more) of the above factors causing the bursitis and deal with each one. This is System 2 thinking.
As you can see, bursitis is not a self-explaining entity and is not a satisfying diagnosis that can be treated with corticosteroids or surgery. Corticosteroids mask the underlying problems and shut down healing processes. Surgery removes an essential structure. This is where functional and integrative sports medicine comes in. Now, we can think about biomechanical causes while we watch the patient walk, thrown or run. We can find out if they need nutritional help, and we can find out what type of physical therapy will help solve the underlying problems. Sometimes, as in my last published case of the youth pitcher, all we needed to do was link the existing coaching information for the patient into a single pitch, and the stress on the painful joint is relieved. Occasionally biologic and cutting-edge therapies may have a role. Integrative medicine takes a multi-disciplinary approach, for a more permanent and natural solution.
To summarize, a functional approach assesses the patient, adds up the underlying causes, and refuses to accept the presenting symptom as the entire picture. It leads to a diagnosis that is more holistic and more specific. The integrative approach then utilizes several treatment approaches to get a much more comprehensive set of treatment options. Integrative sports medicine asserts a true team approach, where the team synergistically employs the available skills, techniques, and treatments, utilizing any or all parts of my skill-set, and most importantly all the therapeutic community.